How the new impatient patient is disrupting medicine
Patient activists have never been as vocal. But are they truly being heard?
Jennifer Kravis and Sue Faber prepare for their meeting with the Minister of Health in Ottawa to discuss Lyme Disease. (Photograph by Jessica Deeks)
Share

Updated March 28, 2018
In late August 2017, Sue Faber and Jennifer Kravis hauled close to 150 pounds of documents and scientific research into a Health Canada office in Ottawa. The two women, co-founders of Lyme-patient advocacy group LymeHope, had been granted a 15-minute audience with then federal health minister, Dr. Jane Philpott, and Dr. Theresa Tam, head of the Public Health Agency of Canada. They’d lobbied hard for the face time and intended to make the most of it.
Faber, a former registered nurse who lives in Burlington, Ont., and Kravis, an Oakville, Ont.-based lawyer who’s not currently practicing, call themselves the “Lyme Moms,” a folksy moniker that belies their organizational and research skills. The two suitcases they rolled into the room contained months of work: a petition circulated online calling for urgent government action signed by more than 47,000 Canadians; 2,700 letters, organized by province, from people sharing their harrowing experiences with the bacterial infection spread by ticks; and binders of published research.
That Canada’s top health officials spared even 15 minutes to meet with civilian advocates reflects the current medical moment, one in which patient activism appears to be driving the medical status quo, with “patient-based medicine” and doctor-patient “shared decision making” the new buzzwords.
Examples of patient groups driving the agenda abound—from the push to legalize medical marijuana to the right to assisted suicide. It also underlines the federal government’s $4-million “Framework on Lyme Disease” introduced in the spring, mandated by Green Party leader Elizabeth May’s Bill C-442 which was passed unanimously in 2014. May, who calls Lyme “a national emergency” given rising incidence due to climate change, inaccurate testing and treatment protocols, credited patient advocates for the bill’s passage. Likewise, people with MS pressured the federal government to sponsor a $6-million clinical trial into treatment for a newly classified venous condition, dubbed CCSVI, shown in an observational study and YouTube testimonials to benefit some people with MS, against recommendations of the Canadian Institutes for Health Research (CIHR), the MS Society of Canada and MS neurologists.
It’s a landscape in which the very word “patient” — derived from the Latin “patior,” to “to suffer, experience, or endure” — is an anachronism. In a recent video for NEJM Catalyst, “What if our care were designed by patients?” American radiologist Stephen Swensen suggests “patient” be replaced by “people,” as it’s more “humanizing.”
But that word doesn’t capture the new wave of patient advocates, represented by Kravis and Faber. With their access to medical research, medical professionals and social media mobilization, they’re more accurately “impatients.”
Closer examination of recent patient activism, however, reflects a more complex story—systemic failures, establishment backlash, and evidence the mandate to “listen” to patients doesn’t always mean they’re being heard. The medical establishment is quick to point out that the Internet can put users at risk. With its echo chambers, social media can abet “confirmation bias,” seeking information that reinforces one’s beliefs. Bad and false science can readily be spread, seen in the rise of the anti-vaccine movement and on Gwyneth Paltrow’s Goop.com.
But the Internet has also brought a more positive sense of connection between previously isolated people who share a diagnosis—as well as channels to exchange information and mobilize, which in turn has given patients a greater voice in decision-making. Elizabeth May, for instance, called for patients to have input into creation of the Lyme “action framework.” That didn’t happen. Recently, an Alberta government official came forward to say the “patient experience” surveys, intended to gauge patient satisfaction as well as areas needing improvement, aren’t being used. Such data is only valuable if it’s acted upon, Stafford Dean, chief analytics officer for Alberta Health Services, told HealthyDebate.ca in September. Currently it’s not, he says: “Bottom line, we’re not actively managing or trying to move these patient experience measures….It’s all passive improvement.”
It’s a shifting landscape in which tensions run high and questions remain. How to base patient demands on “evidence-based” science? How will the changing role of patients affect doctors’ roles? Who decides healthcare spending? And, ultimately, who tells the story of disease?
Surges in patient activism, and the rise of patient rights, have historically mirrored societal shifts. The first patient-led societies, the National League of Blind People and the National Association for the Deaf and Dumb in the 1880s, occurred alongside the rise of the British labour movement; the civil rights’ and women’s movements of the ‘60s saw a concomitant recognition of patient rights; now, the current Internet-driven iteration is proving the most seismic yet.
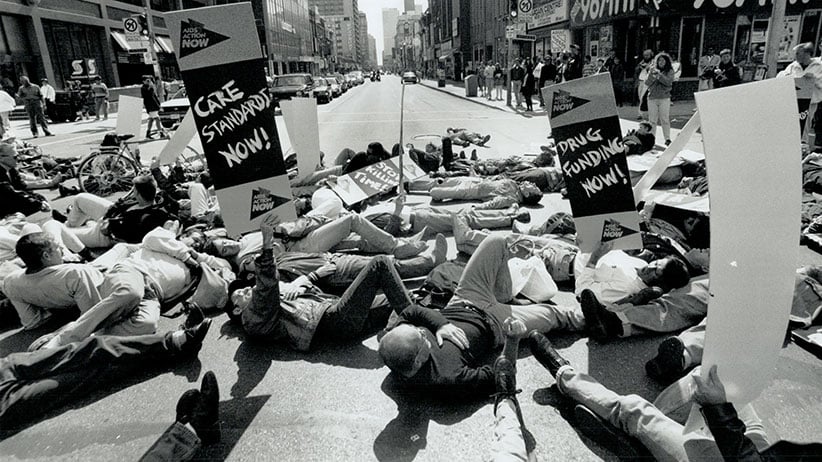
HIV/AIDS activism in the ‘80s brought “patients” into the political/policy realm. These activists introduced the concept of a self-educated ‘disease constituency’ able to critique and challenge the medical establishment in its own language, Steven Epstein writes in Impure Science: AIDS, Activism and the Politics of Knowledge. The FDA altered drug efficacy criteria to fast track AIDS drugs to market as a result.
The arrival of ‘80s neoliberalism transformed patients into “stakeholders” with a right to sit “at the table”; they became de rigeur on research review panels, ethics and drug policy committees, health-policy conferences, and the like.
The right-to-die movement is tethered to the rise of patients’ rights, notes Sandra Martin, author of the 2016 book A Good Death: Making the Most of Our Final Choices: “People have always asked their doctors for help in dying. And doctors have complied, but out of compassion, not a sense the patient had a right to ask for help.” Martin draws an analogy with “consumer advocacy,” though cautions the comparison is imperfect. “These are rights we’re entitled to,” she says. “Patients want to be able to say ‘I’ve had enough. I don’t want another chemo round’.”
The desire for personal testimony, in memoir and later blogs, has factored too. Suffering commands attention and compassion, even credibility, witnessed in how a letter written by 84-year-old Gillian Bennett, diagnosed with dementia who died of suicide in 2014, rekindled the assisted suicide debate. “People want to get their message out as a legacy,” says Martin.
In that regard, the Internet and social media have delivered tools to detonate what Canadian psychiatrist Norman Doidge calls “the military metaphor of medicine” — one in which the patient is “merely the passive battleground where the two antagonists, the doctor and the disease, fight it out.”
In 1998, PubMed.gov went online, giving the public direct access to biomedical research. People once homebound and invisible were able to form online communities — to share experiences, rate their doctors, even discuss participating in clinical trials, formerly a taboo topic. Chatrooms and Facebook pages became places to mobilize, to circulate petitions, and to exchange research that ran contrary to medical dogma.
That was the story of CCSVI advocacy which was inspired by research conducted by Paolo Zamboni, an Italian vascular specialist working outside of the multiple sclerosis establishment. Zamboni identified patterns of extracranial venous blockages in people with MS and found, in a small observational study, that venous angioplasty reduced and even eliminated MS symptoms. Joan Beal, a Los Angeles-based opera singer who had been investigating vascular links to MS after her husband, music composer Jeff Beal, was diagnosed with the condition in 2007 forwarded Zamboni’s study to doctors at Stanford University. Michael Dake, an interventional radiologist, saw its merit and performed the treatment on Jeff Beal. His positive post-treatment results, shared online, spurred people living with the incurable, degenerative disease to seek the procedure offshore, contrary to their neurologist’s advice. Results, shared on social media, indicated the procedure worked for some, but not for others. Media coverage put the spotlight on the conflict, one that saw fault lines grow between people with MS, MS neurologists and MS societies who rejected Zamboni’s hypothesis. The ensuing fallout saw some MS patients sever relationships with their doctors to form their own groups that held conferences to discuss new scientific research that wasn’t receiving mainstream attention. Joan Beal would go on to become a leading proponent of a new vanguard of emerging scientific research unearthing links between the vascular system and neurodegenerative diseases.
The concept of “patient-based” medicine should be a redundancy. In the late 19th century, Sir William Osler, a Canadian physician and founding professor at Johns Hopkins Hospital, famously advised students to “Listen to your patient, he is telling you the diagnosis.”
More than a century later, in 2011, the CIHR initiated a strategy for “patient-oriented research” (SPOR) to make patients “active partners” based on the recognition “patient-identified” priorities are seen to “improve patient outcomes.” In August, Dr. Laurent Marcoux, incoming president of the Canadian Medical Association, told doctors they must serve patients “first and foremost,” an instruction that should not be necessary: “We have to put the interests and the needs of our patients as a whole before our own,” he said.
It’s an instruction that reflects deeper health care malaise. SPOR’s creation, the CIHR website notes, was in response to the finding that 50 per cent of patients don’t receive treatments of “proven effectiveness” and up to 25 per cent get care that isn’t necessary or is potentially harmful. Marcoux pointed out that people are receiving needless tests under the false belief early diagnosis is beneficial: “We think it’s better, but it’s not,” he said. Likewise, in his video calling for a more emphatic doctor-patient relationship, Stephen Swensen says that could result in more patients taking their meds; the lack of trust in doctors has led to a third of prescriptions handed out by U.S. doctors not being filled, he says.
The fault lines are laid out by Dr. Joel Lexchin’s in his book Doctors in Denial: Why Big Pharma and the Canadian Medical Profession Are Too Close for Comfort. The physician and professor emeritus at the School of Health Policy and Management at York University, outlines a system in crisis — healthcare spending under pressure, a flat CIHR budget, and increasing industry-funded research and influence. The interests of industry, directed to maximize profit, are diametrically opposite to those of public health and patient care, Lexchin writes.
There’s no more damning sign of crisis than the rise of a “patient advocate” industry, in which private advocates are paid to help patients and their families navigate Canada’s labyrinthine healthcare system.
The newfound influence of patient-based groups is also reflected in the fact drug companies are targeting them much as they did physicians and medical groups — to increase their influence with governments and to market products. It’s a phenomenon charted in Advocacy Inc.: How Pharmaceutical Funding Changed the Breast Cancer Movement, by Sharon Batt, a former patient activist who teaches in the Department of Bioethics at Dalhousie University. Batt describes the uneasy alliance between industry and patient groups, outlining how patients’ best interests are compromised.
No disease is historically more indebted to patient activism — nor as riven by patient-doctor friction — than Lyme. It was research by two intreprid mothers, Polly Murray and Judy Mensch of Old Lyme, Conn., not by scientists or doctors, that put Lyme on the map in 1975. Murray began investigating when her four sons and husband experienced mysterious joint pain, headaches, fatigue and neurological symptoms. The women created a data registry of 250 children initially diagnosed with “early onset juvenile arthritis” that was later reviewed by the CDC. Borrelia burgdorferi, the spirochete that causes Lyme, was identified in 1982.
The timeline of Lyme advocacy dovetails that of HIV/AIDS, says Holly Ahern, associate professor of microbiology at SUNY Adirondack, N.Y. Ahern began researching Lyme after her daughter fell sick in 2010 as a college student. The year it took to receive a diagnosis as “a nightmare,” Ahern says, with doctors suggesting symptoms that included joint pain, crushing fatigue and neurological symptoms were psychosomatic: “One said it was because she was ‘a girl under pressure at school’.”
The experience alerted Ahern to longstanding conflict over Lyme between two factions: the Infectious Diseases Society of America (IDSA) which sets guidelines followed by the CDC and most Canadian practioners, and the International Lyme and Associated Diseases Society (ILADS). The IDSA maintains that Lyme is difficult to catch, usually identifable with a bull’s eye rash, and easily cured with a few weeks of antibiotics; persistent symptoms are known as “post-treatment Lyme syndrome; it warns long-term antibiotic use is dangerous. ILADS maintains Lyme can be chronic, which requires long-term antibiotics; a bull’s eye rash is usually not present; the complex bacteria can form biofilms and enter a dormant state, evading antibiotics; other tick-borne coinfections are often present and need to be treated.
Ahern’s research revealed a medical crisis, she says, adding that the ISDA’s approach to Lyme is grounded in “anchor bias” in which early published studies by eminent researchers remain the most influential.
In 2012, she co-founded Lyme Action Network, an advocacy group. New York state has passed a series of bills to deal with the mounting threat of Lyme, she notes, with a Congressional group formed to reevaluate the science. Patients are expected to be at the table.
Not all doctors want to see them there. Washington, D.C.-based rheumatologist Arthur Weinstein, who sat on panels that approved the original Lyme guidelines, gave a presentation at a University of Toronto medical school reunion last May, titled “Lyme Disease: the Facts and the Fiction.” One slide pinpointing areas of activism in the U.S. was disparagingly titled “Lyme Fuss;” another, which referred to the Kravis/Fabers petition, “Be Concerned About Public Education and Government Affairs petition.”
Weinstein expresses concern about “naïve politicians” wading into medical issues under the influence of such pressure. In an email to Maclean’s, he said, “My experience has been that they are swayed by the emotional pleas of the patients and advocacy groups rather than scientific truth.”
Certainly successful advocacy can skew resources irrationally. A 2011 study by Charity Intelligence Canada identified that 47 percent of the cancer charity funding in Canada goes to breast cancer, 38 percent to children’s cancer, and 8 percent to prostate cancer. That leaves the remaining 7 percent for all other types of cancer, including some of the deadliest and most prevalent, such as lung, liver, and colorectal.
Forty years after the first “Lyme Moms,” Kravis and Faber went to Ottawa to lobby for Lyme patients. The two women refer to themselves as “accidental activists,” spurred by their Kafka-esque experiences with Lyme. In 2016, Faber and one of her daughters tested positive for a European strain of Lyme in Ontario (her two other girls are also afflicted); Kravis suffered five years of debilitating symptoms that forced her to leave an executive position at a bank; she was diagnosed in the U.S.
Both women sought long-term antibiotic treatment in Canada, but ended up travelling to the U.S. After two years of intensive antibiotics, Kravis says, her stamina and quality of life improved. Like Faber, she never saw a rash. Lingering symptoms remain, she says, including severe muscle and joint pain, insomnia and fatigue. It wasn’t a cure: “I missed the early window.”
Both women also express frustration that the government didn’t consult with Lyme patients when creating the Lyme “framework,” despite a three-day government-sponsored conference in May, 2016; 360 of the 581 attendees online and in person were patients, caregivers or members of patient groups.
Weeks later, HealthyDebate.ca, the sponsors of which include the CIHR, ran an opinion piece arguing that Lyme patients should not be equal partners in policymaking. The recommendations made by patients at the conference were based on “controversial and unproven claims,” authors Melanie McPhail and Jacob Shelley argued, warning U.S. advocates convinced legislators to allow long-term antibiotic use “despite a lack of credible evidence.”
Shelley, a professor at the Faculty of Law & School of Health Studies at Western University, found the conference frustrating, he told Maclean’s: “Experience of disease was conflated with expertise,” he said. “During patient testimonials, patient after patient got up to say how they’d been ignored by the system, then went on to talk about the 40 or 50 tests they had done and the 30 specialists they’d seen. I say, ‘You’re not being ignored, you’re just not getting the results you want’.”
Philpott acknowledged patient frustration when the framework was announced: “Canada’s medical system has failed Lyme disease patients,” she said.
Kravis and Faber delivered stories from thousands of those patients: adults and children with bull’s-eye rashes being denied treatment; GPs refusing to test because they don’t know what to do about tick bites; anger about new Health Canada/CBSA policy to seize Lyme patients’ prescription drugs at the borders.
They brought with them documentation of how children with possible Lyme are being classified as psychiatric cases and admitted to psych wards, and how parents are being threatened with Children’s Aid investigations for treating kids out of country. They also connected dots, suggesting that undiagnosed Lyme might explain high incidence of mental health, arthritic and chronic illnesses in Indigenous communities which tend to be hyperendemic for Lyme and coinfections.
They left the 15-minute meeting optimistic. Minister Philpott was receptive, they say. They left behind four binders of research, including a 1988 Canadian Medical Association Journal study on transplancental transmission that defies the prevailing view that Lyme cannot be transmitted in utero (the government is planning a literature review into the topic).
Kravis returned to Ottawa in mid-September for a Lyme patient roundtable. They asked that clinicians and scientists with expertise treating Lyme be present but were turned down.
Societies representing patients are scrambling to adapt to the rise in patient advocacy. In 2012, the year the CCSVI clinical trial was announced, the MS Society of Canada invested almost $280,000 of its research money to study CCSVI activism, which upended its research agenda. CCSVI has become both a warning and a cautionary tale of the threat of patient advocacy. Preliminary results from the clinical trial were announced last March. It found treatment for CCSVI “inefficient” for MS. (The complete study has yet to be published.) The CCSVI file should be closed, neurologist Anthony Traboulsee, who led the trial, told CTV News: “It’s done.”
Last month, the study into CCSVI commissioned by the MS Society was published. “CCSVI is a harbinger of insurrection to come,” says the study’s author Michelle Driedger, a professor and Canada Research Chair in Environment and Health Risk Communication, at the University of Manitoba. “It’s going to happen again because we have so many diseases with unmet therapeutic needs.”
The MS Society initially came across “as not being sufficiently responsive to donors or the population group they are intended to serve,” Driedger told Maclean’s. They’ve changed strategy: “There has been more engagement of MS patients — meetings across country to find out what research they’re most interested in.” One offshoot has been a study into nutrition and MS.
Caution is required in a publicly funded system, says Dreidger: “Just because a patient might ‘want’ something, doesn’t mean they should have access,” she says, noting that, for the most part, health-care administrators aim to ensure insured services are supported by evidence.
The public-health researcher points out that having “a seat at the table” doesn’t guarantee participation, or assurances that patient/public experiences will be addressed.” She calls for “a mechanism to engage broad groups of people in more than a tokenistic fashion.”
Most physicians have a hard time trying to implement “shared-decision making” in practice, Dreidger notes. She sees the need to get past “health-system gate-keeping” to ensure that something inherently uncertain isn’t dismissed without consideration to whether or not it could be as plausible an explanation as anything else. This is particularly true of Lyme, which is often misdiagnosed for such incurable conditions as MS, ALS and Alzheimer’s. Last year, 80-year-old singer and actor Kris Kristofferson, initially diagnosed with Alzheimer’s, was tested to find out he had Lyme.
As the patient role changes, so must that of doctor, a word from the Latin “doceo” — “to show, teach, cause to know.” So claimed a 2016 New England Journal of Medicine op-ed, calling for doctors to embrace “medical uncertainty,” the reality that they don’t always know the answer. It’s a concept that runs contrary to the culture of medicine, for both doctors and patients, the authors write: “In medicine today, uncertainty is generally suppressed and ignored, consciously and subconsciously” as it “instills a sense of vulnerability in us — a sense of fear about what lies ahead.”
In the future, “value as physicians will lie in the ‘gray-scale space,’ where we will have to support patients who are living with uncertainty — work that is essential to strong and meaningful doctor–patient relationships.” While doctors grapple with “uncertainty,” patient advocates are funding research themselves. The California-based Bonnie J. Addario Lung Cancer Foundation, a “patient-founded, patient-focused, and patient-driven” organization, recently released a report celebrating the fact patients sharing a specific genetic mutation are connecting online to form groups to fundraise and advance research for their specific cancer subtypes. Laura Greco, a stage IV non-small cell lung cancer patient, a member of “ALK Positive” which raised $120,000, expressed frustration that the research status quo “is not enough to save our lives.” Ross Cambridge, director of thoracic oncology at the University of Colorado spoke of a new patient sensibility: “There’s an element of not just offering yourself up [for research] and having someone then treat you as a piece of meat.”
These collectives also mirror the changing image of cancer — into smaller and smaller molecular subgroups — that drives the new push for genome-based therapeudics. Most of the foundation’s sponsors are major pharmaceuticals.
In Canada, the CIHR is about to put out a call for research submissions on Lyme, with patients being invited to the peer review panel. Meanwhile, the G. Magnotta Foundation for Vector-Borne Diseases donated $1.4 million to a lab at the University of Guelph this June which will research how to improve Lyme testing and treatments. The non-profit was established in 2012 by Rossana Magnotta, CEO of Magnotta Winery, in honour her husband, Gabe, who died in 2009 of complications from Lyme; he’d been ill for close to seven years, four seeking diagnosis as his health deteriorated. He finished aggressive antibiotic treatment out of country in August 2009 and could walk over a kilometre a day. In December, he died of a heart attack. He was 59. “My goal is to solve this problem through evidence-based research,” Magnotta told Maclean’s. Current testing failed her husband and is failing thousands, she says: “Canada should be leading this research but isn’t. They did work on the tick and the bacteria, and surveillance but no money was invested in human tissue research.”
In other words, no money was earmarked for how the infection affects human beings, those people formerly known as patients.
Clarification: This post has been updated to include more context regarding CCSVI advocacy.