Chronic exhaustion, derailed lives and no way out. This is long COVID.
Up to half a million Canadians are suffering from debilitating symptoms of long COVID—and falling through the cracks of a depleted health-care system

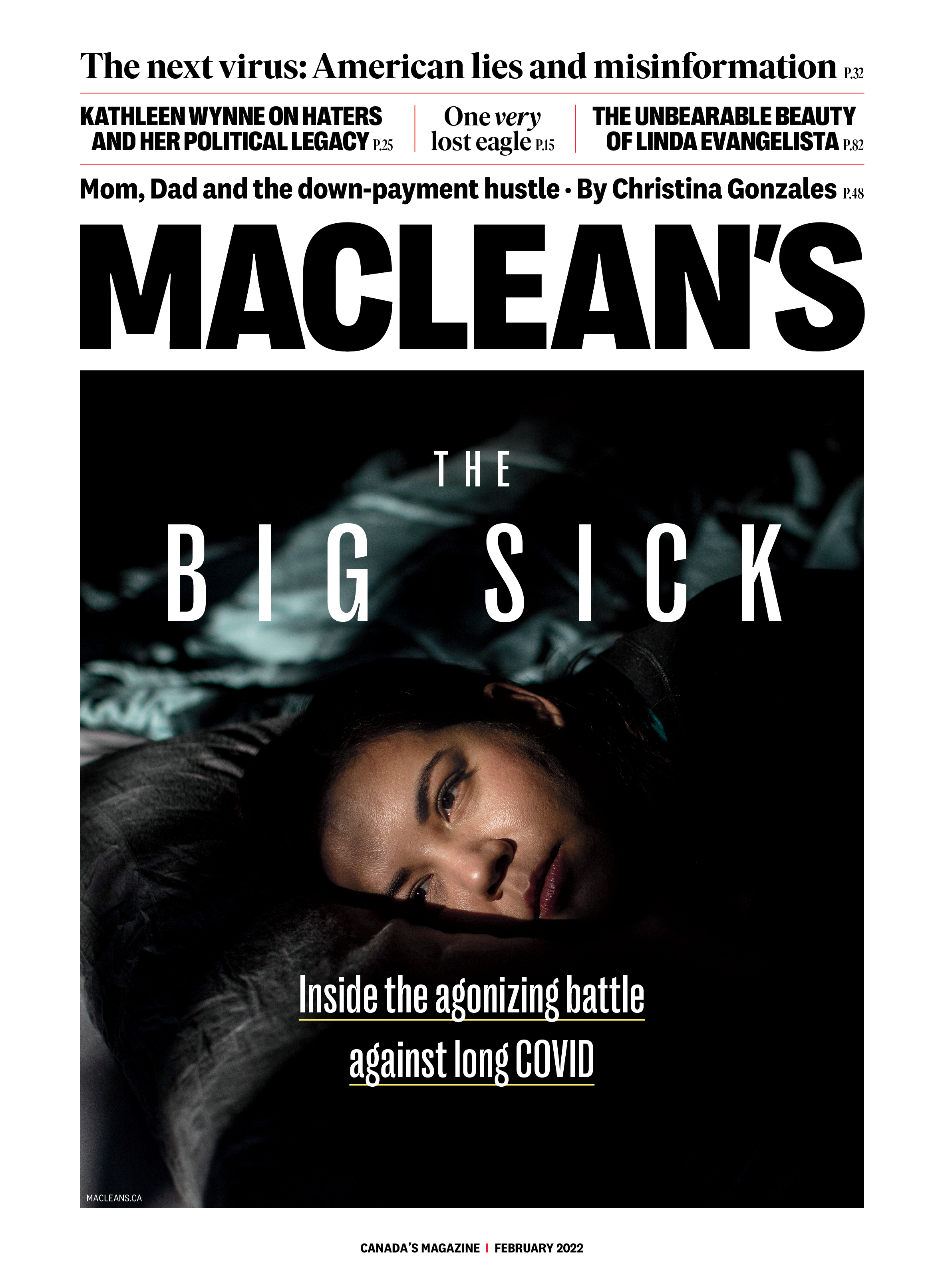
Dr. Daisy Fung: even long COVID patients working in health care are not believed. (Photograph by Jason Franson)
Share
On Christmas morning in 2020, Carrie Anna McGinn woke up in a silent hotel room. There was no little voice squeaking at her to open presents. Instead, her three-year-old daughter was at home, eyeing gifts under a tree at McGinn’s house.
McGinn, 39, a community health worker in Quebec City, was isolating after testing positive for COVID-19. She coughed so much that the muscles around her ribs ached. Standing and talking at the same time was impossible.
She ticked down the days of her isolation, which was scheduled to end on New Year’s Day. By then, she figured, she’d feel better. She would go home and the family could ring in 2021.
But January arrived and McGinn still felt terrible. Some symptoms improved, but many never disappeared, and new issues arose. Almost one year after getting COVID, she still wrestles with a cough, cognitive dysfunction, pain and postural orthostatic tachycardia syndrome, or POTS, which can cause lightheadedness, nausea and a racing heart after she stands up. She has post-exertional malaise, a kind of fatigue that comes on after she’s exerted herself physically or mentally. It can leave her bedridden for days.
READ: First it took his mom. Then his dad. Then, finally, him. The story of a family stolen by COVID-19
“It feels like being wrapped in a lead blanket,” she says. “It kind of feels like my cells are dying.”
After talking to me for about 30 minutes, she begins to cough. “It happens when I’ve been speaking a lot,” she says. The sound reverberates from deep in her chest, as if the basement of her lungs is shaking with the effort to clear what ails them.
***
McGinn has, in the official terminology of the World Health Organization, post-COVID condition. Most people know it as long COVID, a name adopted by patients who became ill in the first wave of the pandemic and never returned to full health. They call themselves long-haulers. The symptoms aren’t the same for everyone, but many experience memory problems, shortness of breath, insomnia, POTS and post-exertional malaise. There’s no set pattern for the course of long COVID: some people are struggling with symptoms that came on while they had COVID, others are dealing with new ones. Some long-haulers say their symptoms fluctuate, alternately improving and relapsing. For some, long COVID is temporary.

Long-hauler Carrie Anna McGinn: 'It feels like being wrapped in a lead blanket.' (Photograph by Chen Zeng)
Many long-haulers had only mild or moderate COVID to start, and were never sick enough to be hospitalized. But their bodies responded to the virus in a way that has left them with prolonged illness and even disability.
Conservative estimates suggest that about 10 per cent of Canadians who contract COVID-19 will suffer prolonged symptoms. Some reports put the number closer to one in three. About 1.7 million Canadians have recovered from COVID-19 so far, which means there could be anywhere from 170,000 to half a million people in this country with lingering health issues from the virus. An unknown number are struggling to return to their basic activities of life. “You can be a marathon runner who can’t walk a block,” says Dr. Angela Cheung, a clinician-researcher at University Health Network and a professor of medicine at the University of Toronto who is studying long COVID. “That is scary for many patients.”
Just like the first surge of COVID-19, long COVID took hold in Canada before anyone knew how to treat it. Long COVID, however, has never drawn the attention or the resources of its acute cousin. The long-hauler population has grown, outpacing the services available to them. Patients are looking for help and often coming up short; they feel dismissed and sometimes maligned. Canada’s health and social support systems are not well-designed for people with chronic, complex conditions, particularly one with a host of invisible and subjective symptoms and no definitive test.
There may be a chance to change the trajectories of long-haulers’ illnesses, but timing is key. If this condition follows the path of other syndromes that have arisen in the wake of viruses—for which people wait months and years for informed medical care and support—they could become even sicker in the long term.
***
Long COVID patients told me that their lives have been turned upside down. They can’t parent the way they used to, or go for hikes, or cook extravagant meals to share with the people they love. They spend long stretches of time in bed. Their family relationships have changed; some marriages have ended. In my interviews with them, long-haulers frequently lost their train of thought and searched for the appropriate word as they grew tired. They often relied on notes that they’d written out for themselves as reminders of what they wanted to say. A number had planned their day around our interview—sending their kids out of the home or booking for their most energetic hour, and then giving themselves time to rest afterward.
Many have not gone back to work; some tried and gave up. Nancy Petalik, a teacher in Flin Flon, Man., says she was so worried about losing her beloved job that she returned to school before she felt better and had to lie down on the floor of her classroom in between classes. She cried as she read aloud from a letter she’d written in her journal in August, outlining how she felt. “I might be okay for a couple of hours of sitting up, but then I’m just overwhelmingly heavy and it’s hard to move,” she wrote. “I crash.” Many people used this term to describe being so sapped of strength that they can’t get out of bed.
People across Canada told me similar stories. Cindy McLean, a pharmacist in the 2,000-person town of Watrous, Sask., got COVID in January 2021 and is still not back to work full-time. She works 10 hours a week, and never a full day. Susie Goulding in Oakville, Ont., who founded the online support group COVID Long-Haulers Canada, shut down her business as a floral designer; the work was too physically taxing. Pamela Godin, a scientist in Yukon who was studying permafrost degradation, has stopped applying for new research contracts; she can’t deal with the intricate data the way she used to.
Long-haulers come from all income levels and industries. “I am seeing health-care workers,” says Cheung, the Toronto researcher. “I’m seeing taxi drivers . . . Some of these are people I know personally. Before they had long COVID, they were colleagues.”
RELATED: Experts are hopeful the Omicron wave will be short, but fear for health care capacity continues
Studies have found that three out of four long-haulers are women. Most are between 30 and 60 years old. “If you’re a woman of working age and you get long COVID, you are extremely at risk of being driven out of the workforce with almost no support,” says Simon Décary, a professor of rehabilitation at Université de Sherbrooke who studies and treats people with long COVID. Many women do not have full disability insurance because they do not work full-time or they left full-time employment to take care of children. If they’re in relationships, especially ones that are already unhealthy, chronic illness adds another level of tension. Décary worries about their vulnerability to domestic violence. “I’m super stressed for these women with long COVID because I know they will be exposed to a very dramatic situation,” says Décary.
***
McGinn has a master’s degree in community health and works to improve access to health and social services for English speakers in Quebec. After she officially recovered from COVID, she started back part-time, just a few days each week. Every shift consumed all her energy. After a workday, she’d crawl into bed. “I couldn’t do anything. I couldn’t take care of my kid the way I wanted to,” she says. She describes the feeling as being the human equivalent of a phone that can never hold more than a five per cent charge. It doesn’t take much to run a battery down completely if its max is only five per cent.
In April 2021, when COVID cases began to climb again in Quebec, McGinn decided to take a month off. She started to feel better; her battery stayed above zero. It occurred to her that she might never be able to work again.
Long COVID created added strain on her marriage, and McGinn moved out. She shares custody of her daughter. It takes her longer to do basic tasks: she needs more time to make meals because she rests mid-preparation. She recently organized papers into a cabinet, a project that in the past would have taken her about an hour. “It took me five hours,” she says. “I kept having the wrong year in the wrong pile and then having to redo it.” McGinn laughs when she tells me she’s an expert in the games you can play with kids lying down. She and her daughter play doctor; her daughter pretends to treat her mom while her mom genuinely rests.
McGinn’s family doctor was supportive but didn’t know much about long COVID and its associated symptoms. McGinn turned online for information and discovered thousands of patients describing remarkably similar symptoms to hers. Some had long COVID and others had a condition known as ME/CFS, or myalgic encephalomyelitis/chronic fatigue syndrome. Some have both.
READ: Inside the murky, high-stakes investigation into New Brunswick’s mystery illness
ME/CFS’s most notable characteristic is enduring and disabling fatigue. People with ME/CFS, the vast majority of whom are women, were dismissed, even scorned, for years. Physicians said their problems were primarily psychological; journalists, writing in the mid-1980s, popularized the term “yuppie flu” to describe their illness. Guidelines released in 2007 recommended that patients with ME/CFS receive cognitive behavioural therapy and graded exercise therapy, a regimen of ever-increasing physical activity. So doctors encouraged patients to find a solution in gyms and therapists’ offices rather than medical clinics. This had a double-whammy negative effect: patients felt scorned by the house of medicine and also suffered from its advice. When they turned to exercise, some patients were overcome with post-exertional malaise. The exhaustion could go on for days, weeks or longer. In a study from the U.S. National Institutes of Health published in 2019, ME/CFS patients reported that exercise, compared to activities like grocery shopping or going to the doctor, triggers post-exertional malaise that comes on faster and lasts longer.
Sabrina Poirier, a 41-year-old mother of two in Halifax with ME/CFS, says she spent years feeling like she was failing because she wasn’t getting better, even though doctors kept telling her she should be getting better. She became suicidal around 2017. She paid privately to travel to the United States and see an ME/CFS specialist. It was the first time anyone told her that her disease was biological, and that there were treatments and approaches she could try, including “pacing” her activities so that she doesn’t overexert herself. It’s a technique that patients use to monitor their energy level so they don’t do more than their bodies can handle.
“I felt a little filled with rage at the Canadian health-care system because I could see where some of the gaps had been, where some of the wasted time had been,” says Poirier, a long-time advocate for ME/CFS patients in Canada.
Although there’s no known cause for ME/CFS, it’s widely believed that an infection can trigger the illness. Many viruses in history—including SARS, Epstein-Barr, Ebola and West Nile—have been linked to fatigue syndromes that arose in their wake.
ME/CFS and long COVID are not the same thing. For one, ME/CFS requires patients to have been ill for at least six months. And long COVID is an umbrella term that covers a broad group of patients. But the two conditions have overlapping symptoms: fatigue, post-exertional malaise, POTS. Now that long-haulers are reaching the six-month marker of illness, some meet the criteria for ME/CFS, too.
Dr. Amir Landi, a physician turned scientist at the University of Alberta, began researching ME/CFS around 2009, after reports that a virus called XMRV could be a cause. The theory is now discredited. Once the XMRV buzz died down, Landi, an immunologist, was one of few scientists who remained focused on ME/CFS. Landi calls a 2019 ME/CFS grant from the Canadian Institutes of Health Research the first major recognition in this country that the syndrome could have “biological backbones.” He says years of research into post-viral syndromes were lost because ME/CFS was downplayed and patients were not believed. “The patients were mostly considered psychological, malingering in their heads,” he says. But that was wrong, says Landi; while many ME/CFS patients do have anxiety and depression, it’s often in response to the life upheaval from their illness and not a primary cause.
Patients with ME/CFS and long COVID are still bumping up against the idea that their illness is psychological, or imagined, or exaggerated. Dr. Daisy Fung, a family physician in Edmonton and an assistant clinical professor at the University of Alberta, got infected with COVID in March 2020. After a week of blisteringly high fever and pain, she improved. She still felt more tired than usual, but the mother of four figured she was feeling the pressure of working as a long-term care physician during the pandemic. In late 2020, she became a surrogate for a friend and felt good during the pregnancy, but after having the baby in the summer of 2021, fatigue and pain hit her full blast. (The immune system changes during pregnancy, and Fung thinks this may have buffered her from some of the long COVID symptoms.) To preserve her energy, she stopped teaching and revised her clinical practice. She now has a schedule that allows her to nap during the day if she needs to.
This summer, Fung spoke out on social media about being a physician with long COVID and was surprised by the cruelty of some of the responses. She says a psychiatrist reached out to tell her that her problems are all in her head; another physician told her that she’s not fit to practise medicine. She is distressed at how often patients with long COVID, even those who work in health care, are not believed. “We have continued beliefs out there in the profession that long COVID is not real, and fibromyalgia and chronic fatigue are not real,” she says. “It’s very minimizing and invalidating to hear that from my own colleagues. If that’s how they’re talking to me, what are they saying to patients?”
Some of the longest long-haulers in Canada are health-care workers who were sickened in the first waves of COVID. As patients, they find they’re sometimes educating doctors and other health professionals on how to care for them. Alyssa Minor, a physiotherapist in Calgary with long COVID, says she’s privileged to have a family physician who’s supportive and willing to listen to her ideas. “But I come with the ideas,” she says. Minor worked with acute-care patients in hospital, many of them with COVID-19, before she tested positive in January 2021, one day before she was due to receive her first vaccine dose.
In her year with long COVID, she’s been frustrated by the lack of knowledge that many physicians and health-care workers have about the illness and its related symptoms. Minor was referred to a cardiologist for tests, including 24-hour Holter monitoring, an echocardiogram and a treadmill stress test. When it came to the treadmill, she found herself trying to weigh the benefits of having the test results in hand versus the potential risk that the test would cause her to crash. She asked the cardiology team about their protocol for patients with post-exertional malaise. After learning they didn’t have one, she asked them to consider other test options for patients being sent to them with symptoms related to long COVID and ME/CFS. “I wrote down stuff for them and said, ‘I hope you do something with this.’ ”
***
By the day, the number of people in Canada with long COVID grows. The same cannot be said for the health-care workforce and infrastructure that is available to care for them. In Sherbrooke, Que., Dr. Alain Piché opened the province’s first and still its only long COVID clinic that’s not research-based. He now has a panel of more than 500 patients, with another 150 on the waiting list. “The turnaround time is four to six months now,” he says.
McGinn drives 2½ hours from Quebec City to see him. She and other long-haulers pay out of pocket to stay in hotels before and after their appointments. “I aggressively rest for two or three days to recuperate, to try to not crash too badly,” says McGinn.
In rural areas of the country, patients fall into even larger gaps in the care network. Petalik, the teacher in Flin Flon, was infected with COVID-19 during a large community outbreak last spring. Everyone else seemed to get better except her. Petalik, 55, used to hike in the bush near her home for hours every weekend; now, she is barely able to walk around the block, she says. Once, she almost set the family cabin on fire. She forgot to turn the stove off and she was lying on the couch after dinner when she realized her eyes were stinging. With her sense of smell still missing after COVID, she hadn’t noticed the smoke coming from the stove.
When she called her family doctor, the physician told her that she didn’t know what was wrong. Through online support groups, Petalik found the Bourassa Clinic, a rehabilitation clinic five hours away in Saskatoon that provides multidisciplinary care for long COVID patients. It’s out of province but closer than Winnipeg, the next major centre, which is eight hours by car. Petalik’s husband drives her to appointments, and they stay with their daughters in Saskatoon. Her insurance covers about $300 in physiotherapy for the year, which she’s burned through. The couple has paid out of pocket for transportation, assessments and physiotherapy.

Teacher Nancy Petalik; women with long COVID risk being driven out of the workforce. (Photograph by Carey Shaw)
There are glimmers of hope. Petalik says she’s improved with the physiotherapy. She can walk through Walmart and the grocery store, things she couldn’t do last summer. She’s careful about pacing and monitoring her energy so she doesn’t crash. She feels like she’s on the road to recovery, and her employer has been supportive, she says.
McGinn, who runs a long COVID support group in Quebec, says long-haulers often talk about a lack of income support. People who have disability benefits are the lucky ones; others are paying out of pocket and chewing up their savings, or continuing to push themselves to work. “I see people falling through the cracks of the health-care system and falling through the cracks of the financial support nets that could be available to them,” she says.
MORE: Misinformation from the U.S. is the next virus–and it’s spreading fast
It takes time to process documents for short- and long-term disability. Goulding, who founded the COVID long-haulers support group, would like to see a kind of episodic disability insurance available to long-haulers, reflecting the non-linear trajectory of their disease. And she’d like these supports available without proof of a positive COVID test, which many people, including Goulding, do not have. She became sick in March 2020, when testing was limited to health-care workers and travellers.
With so many holes in the system, patients are turning to each other. In online support groups, they share information on research studies and ask questions about navigating the bureaucracy around financial support. Long-time ME/CFS patients, like Poirier, serve almost as ambassadors or mentors.
Minor, the Calgary physiotherapist, says she’s grateful for the people in the ME/CFS community who’ve been advocating for years. When Minor walks into a room as a patient, she tries to return the favour. She thinks about representing all the patients who don’t have the disability coverage or the health expertise that she has. “[I imagine that] I’m never alone in that room,” she says.
***
Fortunately, long COVID holds one huge advantage over the many post-viral syndromes in the past: the sheer number who are being closely documented and researched around the world. Cheung, who is leading a major Canadian study of long COVID called CANCOV, points out that ME/CFS patients are rarely diagnosed within the first two years of illness, so it’s not always clear what triggered their disease and what happened in the early stages. With long COVID, though, things are different. Many people know that COVID sparked their prolonged illness. They began receiving treatments in the form of physiotherapy, rehabilitation and medications earlier in their disease process, and they are being followed in studies around the world, making them the largest documented cohort in history of people with a post-viral syndrome. “I’m hoping that because we pick them up earlier, we can do things to alter their trajectory and recovery,” says Cheung. She encourages people in Canada with long COVID to participate in research studies wherever they can.
She says people with long COVID shouldn’t lose hope. She is seeing positive outcomes in patients. “I do see people getting better,” she says. Early results from CANCOV indicate that resting and pacing can help with fatigue and prevent crashes, and breathing exercises can strengthen the muscles around the rib cage to help with ongoing respiratory issues. She sees that patients are frustrated because they want answers, and physicians don’t have them. The lack of knowledge about their disease is compounded by Canada’s ongoing shortage of mental health services that could support people with anxiety, depression and fear related to their illness, she says.
The scale of the problem is almost too monumental to grasp but, equally, too monumental to ignore. Décary has examined long COVID models around the world and advised Alberta Health Services on its strategy, and he has a wish list for how to change Canada’s approach. First, he says, every province should create a centralized system to get patients assessed and into a care pathway designed for them. “It’s such a complex disease that a simplified intervention does not work,” he explains. Patients need time with physicians, physiotherapists and rehabilitation specialists, but Canada’s current system is not designed for long visits.
Second, Décary says, provinces need to support and invest in primary care providers to improve their knowledge about long COVID. The model of long COVID clinics will not be sustainable on the scale that’s needed, he believes. Long-haulers will require care for years, not months. That’s best accomplished through primary care. Third, patients need to be connected to long-term rehabilitation services, just like stroke patients or those with other complex diseases. Décary says the most efficient option is through public-private partnerships. Finally, patients need to have smooth referrals for specialty care when they need it. There are too many barriers right now for patients to see pulmonologists, cardiologists, immunologists and others. And, he says, this model should be available for any patient with a complex disease, whether it’s long COVID, ME/CFS, chronic pain or fibromyalgia.
Patients like McGinn don’t have time to wait. She’s getting ready for what might lie ahead. She believes she’s likely to be diagnosed with ME/CFS because of her prolonged symptoms. Based on what she learned from other patients, she has moved into a new home that is adapted for her expected long-term needs. She and her daughter will open gifts together this Christmas in an apartment with no stairs to manage. The building has wheelchair access ramps, elevators and an indoor parking lot, and is close to a primary school that her daughter will be able to walk to eventually. McGinn hopes she’ll be able to walk with her too.
This article appears in print in the February 2022 issue of Maclean’s magazine with the headline, “When the virus moves in.” Subscribe to the monthly print magazine here.