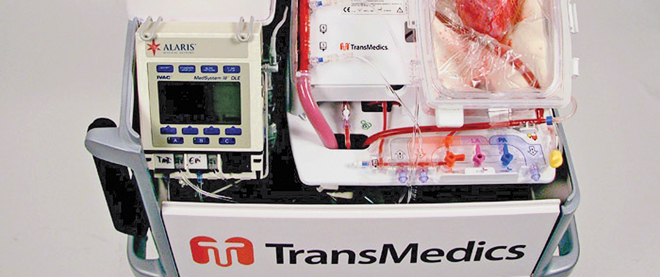
Heart in a box
Will a new technology extend the six-hour transportation time limit for heart transplants?
Photograph by Andrew Tolson
Share
How long can a human heart sit in a cooler of ice—thirsty for vein-borne blood, detached from oxygen and lungs—before it becomes useless to the transplant patient who desperately needs it? Not much longer than six hours, and that’s already pushing it, says Dr. Thierry Mesana, chief of cardiac surgery at the Ottawa Heart Institute. “We don’t have so much trouble with anything under four hours,” says Mesana, who has been transplanting hearts for 25 years. “Beyond six hours is certainly too long.”
Those time restrictions lead to some unfortunate limitations for Canadian hospitals holding patients waiting for heart transplants (as of the end of last year, there were 135 of them in Canada). Even when a perfect match becomes available for transplant, it’s sometimes lost due to degradation over time. Mesana says it’s rare to be able to bring hearts to Ottawa from Vancouver, for example, even when a match—by blood type, age, weight—arises. “We basically can’t do it, most of the time,” he explains. If a match doesn’t turn up within a six-hour radius, the heart is lost.
But the makers of a new technology currently undergoing clinical trial in the United States and Europe say the traditional means of transporting hearts could soon be history. In place of the ice-filled cooler, they promise something seemingly out of science fiction: a box-like machine that carries a beating human heart.
Made by Massachusetts-based TransMedics, Inc., it’s called the Organ Care System. Although not the only such organ transplant system, the OCS is the first to keep the heart warm, and to use an internal, gas-powered pump that causes it to beat more than a litre of the donor’s blood, mixed with a solution of sugars, vitamins, minerals and antibiotics. The technology has attracted media attention, and was even featured in a recent episode of ABC’s hospital drama Grey’s Anatomy.
“The standard of care over the last 20 years has been to pack these things on ice and run as fast as you can,” says company spokesman and head of marketing Neal Beswick. “It limits how far you can reasonably travel.” But Beswick claims the OCS will help prolong the heart’s longevity from the time it’s removed from the donor to when it’s transplanted into the recipient. “In a way, we freeze time for the heart,” he says.
So far, 125 people in the world have received hearts transported by an OCS. The longest any of those hearts was ever outside a human body was eight hours, says Beswick. It was transported from Greece to Berlin. Even so, in light of animal testing conducted by the company, Beswick is confident the system could support a heart for more than 12 hours.
That’s an appealing notion for doctors like Mesana. “I think it’s particularly relevant in Canada,” he adds, given that it’s a geographically enormous country with a widely dispersed population. Because the OCS monitors the performance of the heart during transportation by allowing doctors to review information on a wireless monitor, Beswick says it can help keep bad hearts from being transplanted, thus increasing survival rates and positive outcomes for patients. That, too, would be a good development, says Mesana. “Anything we can do to protect the heart—and still perfuse the heart and keep it beating during the transportation—may increase our chances,” he says.
All the same, Mesana is hesitant to give his full support to the system until benefits claimed by TransMedics are proven. “Nothing is white and black in medicine,” he says. “We need to see what is really the benefit to the patient.”
Vivek Rao, a doctor and researcher at Toronto General Hospital, is concerned that organ transplant systems like the OCS may have “detrimental effects” on the transported hearts, even if they don’t turn up for several years. “My fear is that these hearts are going to start showing problems at three to five years,” Rao says.
His major concern is that when the donor dies, chemicals are released from the brain into the blood stream. Since the OCS uses this blood to pump through the heart during transportation, Rao worries the brain-death chemicals may cause damage.
Although he admits that the OCS could be beneficial for some patients, he argues that it would only be of help to a minute fraction of the roughly 50,000 Canadians who undergo heart failure every year—something like 70 to 80 people, says Rao. In his view, there is no need to extend the out-of-body life of a heart. For Rao, it’s much safer—in light of his scepticism about TransMedics’ claims—and more practical to turn to ventricular assist devices (VADs), which use spinning rotors to propel blood through the body when the heart can no longer fulfill its function. They remain in place until a matching heart that can be transported to the patient within the existing six-hour time limit becomes available. “We can wait for the perfect heart,” Rao says. “We don’t have to take a heart from six hours away.”
When TransMedics began looking for hospitals to conduct its clinical trial, Rao told the company that, as he was sceptical, he would like to participate. But he was turned down. “They were less than enthused about me investigating the potential detrimental effects of their system,” says Rao.
But Beswick says such criticisms are ill-founded, pointing to the 125 heart transplants that have used his company’s OCS. “We’ve never seen a problem.”
Rao claims an OCS costs about $150,000, but Beswick says that’s not true. Instead, he points to the price in Europe, where TransMedics charges 35,000 euros (close to $49,000) for every heart transplanted with an OCS. Beswick admits that sounds like a whopping sum, but he says, considering what you’re paying for—a strong, new, healthy heart—it’s clearly worth it. Only time, and the results of the clinical trial, will determine whether he’s right.