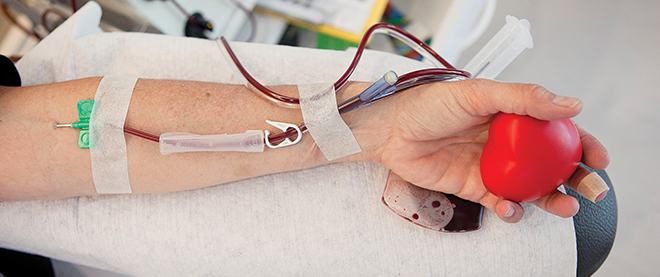
Should we pay for blood?
The prospect of a for-profit plasma enterprise tests the Canadian system
Amaury Miller/Redux
Share
On March 11, federal Health Minister Leona Aglukkaq took to Twitter to issue her first public response to media reports that a private company, Canadian Plasma Resources, had applied to Health Canada for a licence to collect plasma on a pay-for-donation basis. The company appeared confident it would be granted. It had two street-front locations set to open in Toronto, one beside a homeless shelter, and another under construction in Hamilton. Its website, giveplasma.ca, boasted of being “the premier plasma donation location in Toronto.”
Aglukkaq’s first tweet paid homage to the status quo: “Canada has one of the safest blood systems in the world, and I want to help keep it that way.” Her second suggested change was afoot: “I’ve instructed Health Canada to seek the views of people who are interested in the issue of companies purchasing blood plasma.” It also extended an olive branch to Ontario Health Minister Deb Matthews, who only hours earlier had sent her federal counterpart an open letter expressing concern over “the issue of paid donors” and its effect on Canada’s voluntary blood-donation system. She asked the federal government, which regulates blood products collected in Canada, to “refrain from granting approval of any new paid-donor or plasma clinics until there has been an opening consultation with provincial health regulators, care providers, Canadian Blood Services and Canadians.” Matthews indicated that the province, which licenses and regulates medical labs and specimen-collection centres, wasn’t about to green-light the clinics without more consultation.
Days later, in another conciliatory bid, Health Canada convened a closed-door meeting for early April in Toronto, bringing together “stakeholders” in the matter: provincial and territorial governments, Canadian Blood Services, patient groups and the Plasma Protein Therapeutics Association, representing the plasma industry. A press conference originally scheduled to follow the meeting was cancelled; no information on what was discussed, or agreed upon, has been released. The topic, payment for plasma, is divisive: Alberta Health Minister Fred Horne has said his province doesn’t support paying for blood; it’s a non-issue in Quebec, where blood donors cannot be compensated by law.
Canadian Plasma Resources isn’t the first entrant to the pay-for-plasma market; Winnipeg’s Cangene Plasma has been paying for plasma for decades. But it’s proving to be a game changer that’s exposing public interests, political expediency and marketplace realities. Eighty per cent of plasma products used in this country are already produced from paid-for plasma in the U.S. So the real question is: what are the consequences to the Canadian blood system and public health care if Canadian donors are paid for plasma?
The question of blood-system safety remains a flashpoint in Canada, two decades after the “tainted blood” scandal of the late ’80s and early ’90s. More than 20,000 Canadians became infected with HIV and hepatitis C due to improperly screened blood and plasma from paid donors in Haiti and American skid rows. The tragedy led to the creation of Canadian Blood Services and Héma-Québec in 1998, set up to rebuild and oversee the blood system. It also resulted in the Krever commission, which recommended blood donors “should not be paid for their donations, except in rare circumstances.” The World Health Organization agrees: it wants all countries to move to unpaid donation systems by 2020 due to studies pointing to volunteers having the lowest prevalence of blood-borne infections.
But the high demand for plasma is bridging the public and private realms: the viscous, yellow liquid is used both in transfusions and as a raw material for a $20-billion biopharmaceutical sector growing at 10 per cent a year. Fractionation technology separates plasma proteins into life-saving therapies—albumin to treat burns, clotting factor for bleeding disorders and intravenous immunoglobulin (IvIG) for infections and immune disorders. The market for IvIG, in particular, is booming, with Canada one of the highest per capita users. If current clinical trials using IvIG to treat Alzheimer’s are successful, it could result in a new market worth $7.2 billion in the U.S. alone by 2017, Bloomberg News recently reported.
All transfusion plasma used in Canadian hospitals comes from screened, unpaid volunteer donors, says Graham Sher, chief executive officer at Canadian Blood Services (CBS). The country has a surplus of transfusion plasma due to new replacement products and a decline in hospital demand, he says, which led to the agency closing a facility dedicated to collecting transfusion plasma in Thunder Bay, Ont., in 2012. Canada has no fractionation facilities, so CBS sends plasma collected from volunteers here offshore. That meets only 20 per cent of the country’s need for plasma products, he says; 80 per cent is purchased from the U.S., where donors are paid for plasma.
Sher calls treatments made using paid-for plasma “inordinately safe” due to safeguards and the “cleansing” of manufacture. David Page, national executive director of the Canadian Hemophilia Society, cites the industry’s 20-year safety record, a point he made in a public letter released on March 11, the day of Aglukkaq’s tweets. “We maintain that products from paid donors—whether here or in the U.S.—are safe,” Page told Maclean’s. “There’s no way around rigorous standards. Any centre is inspected by Health Canada and the FDA.” It’s “hypocritical” to protest paying for plasma when we already use U.S. product, he says.
But the U.S. paid-for-plasma industry has been criticized for exploiting the poor, with donor sites often located amid extreme poverty—and high drug use. Based on typical industry yields and prevailing prices, it appears that a single plasma donation, for which a donor might be paid $30, results in pharmaceutical products worth at least $300. Unlike blood, which can be donated every 56 days, plasma can be given once a week. Companies and regulators counter that the practice is legal, ethical and safe, noting there have been no known cases of infectious-disease transmission for more than a decade.
Toronto physician Danielle Martin, chairwoman of Canadian Doctors for Medicare, questions for-profit companies collecting and processing blood products: “There’s a potential conflict between the profit motive and the need to maintain the highest possible standards of quality,” she says. She shares Ontario Health Minister Deb Matthews’ worry that a paid-for-plasma system could weaken the volunteerism on which the blood system depends. Sher, for one, says paid-plasma enterprise won’t reduce volunteerism. Data from Winnipeg and the U.S. suggest it isn’t a factor, he says. But other research, including a 2010 report in the Asian Journal of Transfusion Science, suggests otherwise: that study points to the American Red Cross adopting “incentives”—from T-shirts to cash prizes—to spur donations.
Martin also questions the federal government’s lack of transparency on the matter. “They haven’t taken responsibility for an adequate process.”
Matthews told Maclean’s she only learned of Canadian Plasma Resources’ plans shortly before she sent her letter to Ottawa. Yet the federal government has been talking to the company’s principals for four years. EXAPharma, parent to Canadian Plasma Resources, was incorporated in July 2009, a month after a meeting with Health Canada. In November 2010, they registered Canadian Plasma Resources to operate “plasmapheresis centres”; its website went live in March 2011; in November 2012, it applied for a federal licence. EXAPharma is owned and operated by the Riahi family, says Canadian Plasma Resources’ CEO, Barzin Bahardoust. (EXAPharma’s incorporation documents lists Yalda Riahi, a Toronto-area lawyer as president.) A huge investment has been made—from the collection centres to promotional materials to hiring high-profile experts in the field, including former CBS employees and veterans of the German plasma-fractionation industry. EXAPharma plans to produce plasma products through contract manufacturing, then through its own fractionation plants in Canada, says Bahardoust. He’s excited about IvIG, which costs upward of thousands of dollars per treatment: Health Canada and the FDA have approved it for seven indications, he says, but it’s used “off-label,” or at doctors’ discretion, to treat an estimated 300 conditions, including multiple sclerosis. Canada’s high use of IvIG stems from our publicly funded system, he says: “Universal health care provides treatments to anyone who needs them.”
The company plans to pay $20 per donation, but money isn’t mentioned on the website: “As a token of appreciation, we would like to compensate your valuable time and commitment,” it says, suggesting donors give their compensation “to charitable organizations and receive a tax receipt.” In other words, your contribution can still be used to the greater public good.
Company representatives have met twice with Canadian Blood Services: in 2009 and again in 2011 to discuss potential “public-private-sector partnerships,” which included testing plasma at CBS labs, using their storage facility as a backup and referring donors with in-demand blood types to CBS. They also discussed the time frame for CBS’s next tender for plasma-derived products. (The agency awards contracts to manufacturers on behalf of provincial governments.) Sher won’t comment on Canadian Plasma Resources’ business model. “They are not licensed to operate and no commitments have been made,” he says. “Our business model requires that we go through public tendering processes for licensed products that are awarded on safety, security of supply and cost.” Bahardoust appears confident: “As long as our products are licensed by Health Canada, meet the quality standards CBS requires from vendors and are cost-competitive, we’ll be considered as a supplier,” he says. Before that happens, more questions need to be asked.