Heartburn pills that cause heart attacks, antidepressants that lead to suicide
Why does Canada trail U.S. and EU in protecting citizens from dangerous meds?
JENNIFER ROBERTS
Share
On Oct. 17, 2012, Terence Young’s tireless 12-year crusade took him before a Senate committee looking into the safety and regulation of prescription drugs in Canada. The Conservative MP for Oakville, Ont., gave the panel an earful. “Doctors and patients have no way to know when a drug is safe and when it is not,” he argued, noting that his own government’s drug monitoring system is “primarily in the hands of the big pharma companies themselves, even as a growing number of injuries and deaths are reported related to their use.”
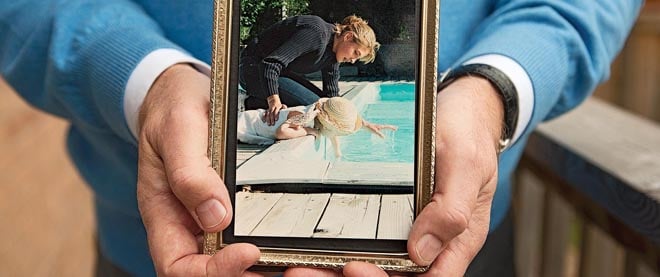
Young was there not as a politician but as a father seeking to redress colossal systemic failure—a mission dating back to March 19, 2000, the day he watched his 15-year-old daughter Vanessa collapse on the floor at home. She was rushed to hospital, where she died a day later. The cause: cardiac arrest.
None of it made sense. Vanessa was a healthy girl. She didn’t drink or smoke or take drugs— with one exception: over the past year, she had periodically taken cisapride, an acid-reflux drug marketed as Prepulsid. Her doctor, who’d diagnosed her with a minor form of bulimia, prescribed it after she complained of reflux and feeling bloated after meals. Neither their doctor or pharmacist mentioned risks; her parents considered it “super Rolaids.”
But when Young dug deeper, he found cisapride was far more toxic than the heartburn it treated: it was linked to 80 deaths in Canada and the U.S. and had generated a total of 341 “adverse reaction” reports in the two countries. More shocking to the former Ontario MPP, Health Canada knew of these risks: since approving Prepulsid in 1990, the agency, which approves and monitors prescription drugs through its Therapeutic Products Directorate, had sent four letters to doctors, the last in 1998, warning about serious adverse effects, including heart risks in children, women and infants.
Had the family lived in the U.S., Young learned, Vanessa might not have been prescribed cisapride. In 1998, the U.S. Food and Drug Administration (FDA) had given it its ominous “black box” warning, an alarm bell that makes doctors far less likely to prescribe a drug. In January 2000, two months before Vanessa died, the FDA issued an advisory alerting doctors of heart attack risks and rewrote label warnings; in April, it announced cisapride would be pulled from the market in July 2000. Health Canada followed suit that May, taking Prepulsid off the market in August.
In 2001, Young marshalled his political connections and demanded an inquest into Vanessa’s death; the 16-day hearing resulted in 59 recommendations, including mandatory reporting of adverse drug reactions by health care professionals and clearer label warnings. A Canadian Medical Association Journal (CMAJ) editorial on the inquest’s findings noted Vanessa’s death was “undoubtedly caused by cisapride” and criticized Health Canada’s response as another example of its “advisory and regulatory actions lagging behind the FDA’s.”
Young also launched a $100-million class-action suit, naming Janssen-Ortho Inc., Prepulsid’s marketer, Johnson & Johnson, its parent company, and Health Canada. And he filed an individual suit against all three parties. The six-year battle, settled out of court, is chronicled in his book Death by Prescription: A Father Takes on his Daughter’s Killer—The Multi-Billion Dollar Pharmaceutical Industry, published in 2009.
His journey into the netherworld of Canadian drug surveillance revealed a system structured to serve the interests of the industry it regulates before the public it’s entrusted to protect. Under the “user-fee” model adopted in 1995, drug companies pay to submit a drug for approval and provide the supporting research. The result is an industry-regulator alliance primed to bring drugs to market. Health Canada has an online database listing adverse reactions to drugs. But navigating it is next to impossible, and reporting adverse effects is voluntary for doctors and pharmacists. Even if a drug is found unsafe, the agency lacks the authority to unilaterally revise the label or remove it from market—or order a company to do so.
Young’s quest to improve drug safety spurred his entry to federal politics. In 2009, a year after he was elected, he tabled a private member’s bill calling for an independent drug-monitoring agency with the power to order unsafe drugs off the market and issue plainly worded risk warnings. It won’t be debated until late next year, at the earliest.
Sitting in his constituency office in October, Young expresses incredulity that prescription drugs aren’t regulated as stringently as other public safety threats: “The minister of transportation doesn’t ‘negotiate’ with truckers to keep unsafe vehicles off roads,” he says. By law, doctors must report unfit drivers, and are paid to do so. Fast-tracking drugs to market is like “air-traffic controllers being told to land planes more quickly,” he says. Eleven years after his daughter’s inquest, none of its major recommendations have been implemented, he says: “Nothing has changed since Vanessa died. It has only gotten worse.”
Vanessa Young’s tragic death thrust her into a big, undiscussed demographic: the 10,000-plus Canadians estimated to die each year from a prescription drug taken exactly as prescribed. And that figure is likely a gross understatement: it is extrapolated from a 14-year-old study, led by University of Toronto researchers and published in the April 1998 Journal of the American Medical Association, that found deaths linked to prescription drugs accounted for some 106,000 fatalities annually in the U.S., making it the fourth-leading cause of death, behind cancer, heart disease and stroke. A 2011 Health Council of Canada study additionally estimated that 150,000 people annually experience serious reactions from prescription drugs.
Those numbers are destined to rise given a market growing by $1 billion a year, according to the Canadian Institute of Health Information (CIHI), which estimates that Canadians spend nearly as much on prescription drugs ($26.9 billion) as on doctors. These medications can improve and save lives. But they’re increasingly prescribed from cradle to grave for an expanding list of syndromes, dysfunctions and disorders—infant reflux, ADHD, adult ADD, social anxiety disorder, female sexual arousal disorder—as well as new health “risks” to manage, such as high cholesterol.
When concerns are raised about prescription drugs, they invariably focus on misuse or abuse: sports doping, OxyContin addiction, teenagers taking parents’ pain meds to get high. That more Canadians are harmed or killed by drugs taken as prescribed than by tainted meat, tainted water and handguns combined is not a blip on the public radar.
But this is changing: a growing number of voices are putting the spotlight on the risks of “proper” drug use. At the Senate committee hearing, Janet Currie, a social worker with the Victoria-based Psychiatric Medication Awareness Group, called prescription-drug side effects “one of the most serious public health problems we have.” Physician David Juurlink, a drug-safety expert and scientist with Toronto-based Institute for Clinical Evaluative Sciences, agrees: “It’s an enormous problem,” he says.
Two new books—Pharmageddon, by Irish psychiatrist David Healy, and Bad Pharma: How Drug Companies Mislead Doctors and Harm Patients, by British doctor Ben Goldacre—present scathing critiques of the $800-billion pharmaceutical industry, including evidence of its routine suppression of negative clinical trial results, something Goldacre calls “a global scandal that puts patients at risk.” The issue was raised in British parliament last month as Conservative MP and family doctor Sarah Wollaston accused drug companies of burying bad news about medicines’ effectiveness and side effects.
Meanwhile, the problem continues to grow. The need for change is reflected in a Canadian study that reveals that serious drug dangers are frequently identified after they come to market. Almost one-fifth (19.8 per cent) of 434 new active substances approved by Health Canada between 1995 and 2010 were later given serious safety warnings—some only months after approval—Joel Lexchin, a physician and professor in the school of health policy and management at Toronto’s York University, found. The study, published last month in the Archives of Internal Medicine, shows risks are higher for drugs fast-tracked in 180-day “priority reviews” (versus the 300-day norm): 34.2 per cent had serious warnings.
Clinical trial results offer a rosy, unrealistic picture of how a drug works, says Juurlink: “In the real world, we don’t monitor people as closely and we don’t select people as carefully. And we don’t apply the same restrictions to a drug’s use.” No one should think a new drug is safe, he says. “Most are overhyped and brought out to maximize appearance of benefit and minimize harm.” Recognizing this, Britain puts an inverted black triangle on new drugs and advises all adverse reactions be reported, says Lexchin: “It’s an extra indication not a lot is known about safety, so be on the lookout.” Pulling drugs from market is rare. One notorious exception was the arthritis drug Vioxx, fast-tracked in 1999 despite known risks; it was removed in 2004 amid a flood of lawsuits after at least 55,000 deaths worldwide. According to Lexchin, only 55 prescription drugs have been withdrawn in Canada for safety reasons since 1963 (Health Canada doesn’t keep track of this data). In comparison, there were 4,852 prescription drugs on the market as of September 2012; 410 new prescription drugs came to market in 2011.
Far more common is a wallpapering of additional warnings that doctors often can’t keep on top of, or find readily on Health Canada’s website. Champix, a popular smoking-cessation drug, for example, was linked to risk of suicide, heart attacks and angioedema, a life-threatening condition characterized by swelling of the skin—all within a year of its 2007 approval. In May 2010, Health Canada and manufacturer Pfizer released a new safety warning telling users with “neuropsychiatric symptoms or behaviours that are not typical for the patient” to stop taking the drug and talk to their doctor. By then, France had stopped insuring it, and doctors in the U.S. were demanding it be pulled from market. In June 2011, Health Canada announced “an ongoing review” that concluded this year with new “precautions for patients with respect to cardiovascular safety.” Even while under review, Champix ads ran with an upbeat “I did it!” tag line, marketing not allowed in the U.S., where stricter rules surround “black box” drug advertising. As of this month, MedEffect Canada’s database lists 1,940 adverse reaction reports for Champix, including 33 “completed suicides.” Yet it’s covered on the formularies of seven provinces, five of which took it on after June 2011.
Drug side effects can end up triggering a “cascade of risks,” says Alan Cassels, a drug policy researcher and professor at the University of Victoria. He points to cholesterol-lowering drugs, or statins, such as Lipitor, Zocor and Crestor, the most widely prescribed drugs in the world. They’re prescribed to manage heart-attack risk, rather than an actual condition, but come with common side effects—muscle pain, anxiety and Parkinson’s-like symptoms—that lead doctors to prescribe additional drugs, with side effects of their own. Cassels wrote of the accumulated risks in July: “Some day, I suspect, we will regard statins as an unmitigated scandal in medicine.”
Eking out patterns of risk is difficult and can take decades, says Juurlink. A study he led, published in the CMAJ in August, tracked 144 patients aged 66 and older who were admitted to Ontario hospitals with acute liver damage; none had a history of liver disease but all had started taking one of five broad-spectrum antibiotics within the previous 30 days. Eighty-eight—61 per cent—died in hospital. The study, which required nine years of data to confirm a pattern, concluded that two specific antibiotics—moxifloxacin (brand name Avelox) and levofloxacin (Levaquin)—“were associated with an increased risk of acute liver injury” in older people, compared with clarithromycin. Hospital records didn’t provide a cause of death, and nobody would think to associate it with antibiotics, Juurlink says. “But I think it’s fair to speculate that the majority of them died of the consequences of their liver injury.” Risks of undetected prescription drug death is highest in older people, he says.
Because deaths linked to prescription drugs are considered to be from “natural causes” in hospital records and coroners’ reports, they’re impossible to trace. That’s something Terence Young wants to change. In 2009, he appeared before an Ontario committee to ask for a new category of death: “related to a medical treatment including a drug prescribed or otherwise recommended by a medical professional.” He was shot down. Coroners can keep drug-related deaths under the radar, Young says: “It’s a conspiracy of silence. They’ve been content to cover up medical errors and harmful drugs for years.”
Yet to hear Health Canada tell it, Canada’s drug regulatory system is not only competent but world-class. Last month, Health Minister Leona Aglukkaq (who declined an interview request from Maclean’s) told the Toronto Star that our drug regulatory system is “one of the safest and most rigorous in the world.”
Many disagree, vehemently. “France and even the United States have regulatory regimes that are much more rigorous and safe,” says Cassels. Juurlink calls Health Canada “a lot of bureaucracy with very little independent action compared to the U.S. and Europe.” The 2011 auditor general’s report criticized the agency for lack of transparency regarding drug approvals, clinical trial data and the status of drugs “approved with conditions,” and for taking years to report safety issues.
The FDA and the European Medicines Agency have made far bigger strides in transparency. In 2010, the FDA adopted “plain language” labelling, something Health Canada has talked about for a decade. The value of clarity is evident in the U.S. monograph for antidepressant Paxil: it refers to “suicidality” at the top in bold type in a black box, plus “risk of increased suicidality” in people under 24 and “the need for close observation.” The Canadian version only starts mentioning anything relating to suicide on page six of its 55 pages.
Extracting information from Health Canada is an exercise in frustration. Drug company information is protected as commercial “trade secrets,” which means it’s withheld from the public. Health Canada spokesperson Sean Upton said many of Maclean’s questions (such as, “How many drugs were approved under ‘priority review’ in 2011?”) would require access to information requests, which can take years, and yield nothing—although he responded a month later saying there were eight. The FDA has the corresponding information on its website, for all to see. Asked what Health Canada did with “adverse effect” reports, Upton responded with boilerplate: they are “systematically monitored to identify rare, new or unexpected adverse reactions,” he said.
Juurlink says that’s a joke. Post-market monitoring of drugs is “a national embarrassment,” he says, calling MedEffect an “electronic dumpster.” As a trained pharmacist, he has trouble navigating it, unlike the FDA’s site. And if reporting of adverse effects by health care professionals was mandatory, as it is in France, Sweden, Spain and Norway, he says, we’d have better data. Cassels estimates 90 to 99 per cent of adverse reactions are never reported.
The lack of transparency runs through the entire drug-approval chain. The FDA, for instance, reveals what clinical trial data was used to support a drug’s approval; Health Canada doesn’t. “It might get a dozen studies and three are favourable and that will be the basis of the approval, but they won’t tell you,” Cassels says. Instead, the agency releases a “summary document” that omits key elements, Lexchin says. “They don’t tell you what trials were submitted, what information confirmed safety and efficacy, the number of people in the trials, the number of subjects who dropped out due to bad side effects.” Data on dropouts is crucial, he says; they’re the first indication that safety problems exist.
Such opacity keeps doctors in the dark, says Matthew Herder, a lawyer and professor at Dalhousie University’s faculty of medicine. In an article published in the CMAJ last year, Herder cites Health Canada’s failure to publicly disclose in 1999 that selective serotonin reuptake inhibitor (SSRI) antidepressants were not authorized to be given to people under 19. By 2004, he notes, SSRIs were widely prescribed “off-label” for teens by physicians who hadn’t been apprised of the risks. Health Canada later claimed the information constituted “confidential” trade secrets, and so couldn’t be divulged by the agency. (“There are no legal boundaries preventing disclosure,” Herder told Maclean’s.)
Health Canada trails regulators in the U.S., Europe, Australia, Brazil and India, who have made registering clinical trials mandatory, a bid to prevent companies from burying negative data. Last month, it announced it was setting up a “web-based list” of Canadian clinical trials—which drew criticism that registration still isn’t mandatory.
“It’s a dysfunctional system,” says physician and pharmacologist Michele Brill-Edwards, who headed Health Canada drug approvals between 1987 and 1992 and quit in 1996 after blowing the whistle on the agency’s suppression of prescription drug risks; she won a 1992 federal court case against her employer. Industry influence only grew as Health Canada switched to the user-fee model in 1995, Brill-Edwards says. Even the language is telling. Internal emails from the period refer to the industry as “the client,” and the job once done by the Health Protection Branch now fell to the mercantile-sounding Marketed Health Products Directorate. A regulator biased to industry interests puts patients at risk, Brill-Edwards says: “The industry’s quest is to get that drug out there and get it used as much as possible. But the more widely we use a drug, the greater the risk that we’re going to end up giving it to people for wrong reasons in ways that will harm them.”
Canada’s small market is a disadvantage when negotiating with industry, she says: “The FDA has a far bigger stick.” But a strong health minister could do it, she says: “You could demand plain-language labelling. They’re already doing it for the U.S. market.”
Drugs produced primarily in offshore factories add another layer of risk, says Cassels, who wrote on the topic in the October 2012 CMAJ. He asked Health Canada about how it monitors this, only to be told it conducted 35 inspections from 2006 to 2011; the agency wouldn’t say which countries were involved or reveal its findings, citing proprietary trade secrets. “That’s a bulls–t excuse,” Cassels says. “Whose team are they on?” He’s doubtful the agency is up to the task, especially after recent budget cuts: “If they can’t or won’t regulate drug advertising, what’s the chance they’ll go to the backwaters of China?”
For now, the task of advocating for better drug regulation continues to fall to those, like Young, whose advocacy is born of tragedy. In November 2010, Nancy and Shaun McCartney’s 18-year-old son, Brennan, went to their family doctor in Bolton, Ont., with a chest cold. The extroverted high school student mentioned feeling sad over breaking up with a girl he’d been seeing for three months. He left with a script for an antibiotic, a puffer— and a sample pack of Cipralex, an SSRI antidepressant. Nancy, a high school vice-principal, expressed concern; Brennan had no history of depression. He assured her the doctor said it would help. On the fourth day taking it, Brennan seemed agitated when he left the house, his mother says. He failed to come home. The next day his body was found. He had hung himself in a local park.
Sitting at their kitchen table, Nancy flips through a binder documenting systemic failure. Brennan wasn’t given the full drug monograph that mentions suicide risk; the sample pack (she has the brochure) notes only “self-harm.” There’s also correspondence with the coroner’s office denying the McCartneys’ request for a toxicology scan. They’ve sent a forensic sample to Australia. “We’ve lost trust in the Canadian health care system,” Nancy says. “Until people have been in our shoes,” says Shaun, “they can’t understand how bad the system is.”
Even their attempts to warn other Canadians about the drug they believe caused their son’s death have been thwarted. After Nancy submitted an adverse-reaction report in April 2012, she noticed a typo on her entry so she called the Vigilance Branch requesting a correction. She also asked for an updated copy. She was told she’d have to file an access to information request. Seven months later, anyone searching Cipralex on MedEffect would find 317 reports, including five “completed suicides,” 12 “suicide attempts” and many references to “suicidal ideation,” but not McCartney’s submission. When Maclean’s asked Health Canada why, Upton responded by email weeks later, saying the entry is in the database, providing a screen grab. Yet subsequent searches using the same terms failed to find it.
“It’s a lot easier to access the system from the inside,” Upton explained. He’s right. And until it isn’t, Canadians shouldn’t believe that our drug-regulatory system is one of the “safest and most rigorous” in the world.